For decades, taking a daily low-dose aspirin was common advice for anyone worried about heart disease. If your parent had a heart attack, your doctor likely told you to pop a baby aspirin. But that advice has changed-dramatically. As of 2025, most healthy adults should no longer take aspirin to prevent their first heart attack or stroke. The science has caught up with reality: for many people, the risks now clearly outweigh the benefits.
Why Aspirin Was Once a Daily Must
Aspirin works by stopping platelets from clumping together. That’s useful when a clot blocks an artery and causes a heart attack or stroke. Back in the 1980s and 1990s, big studies like the Physicians’ Health Study showed that men taking aspirin had fewer heart attacks. That led to widespread recommendations. By 2010, nearly 40% of U.S. adults aged 40-75 were taking daily aspirin for prevention-even if they had never had a heart problem.
But those early studies didn’t account for modern medicine. Today, we have better blood pressure control, more effective cholesterol-lowering drugs like statins, and fewer people smoking. These changes alone have cut heart disease risk by 30-40%. Aspirin’s benefit-about a 10-15% reduction in heart attacks-is now much smaller in comparison. Meanwhile, its biggest risk, serious bleeding, hasn’t gone away.
The New Guidelines: Who Should Still Consider Aspirin?
The latest guidelines from the U.S. Preventive Services Task Force (USPSTF), updated in 2022, are clear: aspirin therapy is no longer recommended for routine primary prevention in adults over 60. For adults aged 40-59 with a high risk of heart disease, it’s a personal decision-only if the benefits clearly outweigh the risks.
Here’s how to know if you’re in that group:
- You’re between 40 and 59 years old
- Your 10-year risk of heart disease is 10% or higher
- You have no history of bleeding problems
- You’re not already on blood thinners
Your 10-year risk is calculated using the ACC/AHA Pooled Cohort Equation. It uses your age, sex, race, blood pressure, cholesterol levels, diabetes status, and smoking habits. Most doctors can run this in under 2 minutes using their electronic health record system. If your score is below 7.5%, aspirin isn’t recommended. If it’s between 7.5% and 10%, the benefit is small and likely not worth the risk.
There’s one exception: people with familial hypercholesterolemia. These individuals have extremely high LDL cholesterol from birth and are at very high risk for early heart disease. Many lipid specialists still recommend aspirin for them, even if they’re under 40.
Who Should Avoid Aspirin Completely?
If any of these apply to you, don’t start aspirin-and talk to your doctor if you’re already taking it:
- You’re 60 or older
- You’ve had a stomach ulcer or GI bleeding in the past
- You take other blood thinners like warfarin, apixaban, or rivaroxaban
- You drink more than 3 alcoholic drinks a day
- You have kidney or liver disease
- You’re over 70-even if you’re otherwise healthy
For people over 60, the data is clear: aspirin doesn’t prevent heart attacks enough to justify the bleeding risk. A major 2018 study called ASPREE followed nearly 20,000 adults over 70. Those taking aspirin had the same number of heart attacks as those taking a placebo-but more major bleeding events, including brain bleeds and fatal gastrointestinal bleeds.
Even if you feel fine, bleeding doesn’t always come with warning signs. Some people don’t realize they’re bleeding internally until they collapse. Others notice nosebleeds, bruising easily, or dark, tarry stools. These aren’t normal. They’re red flags.
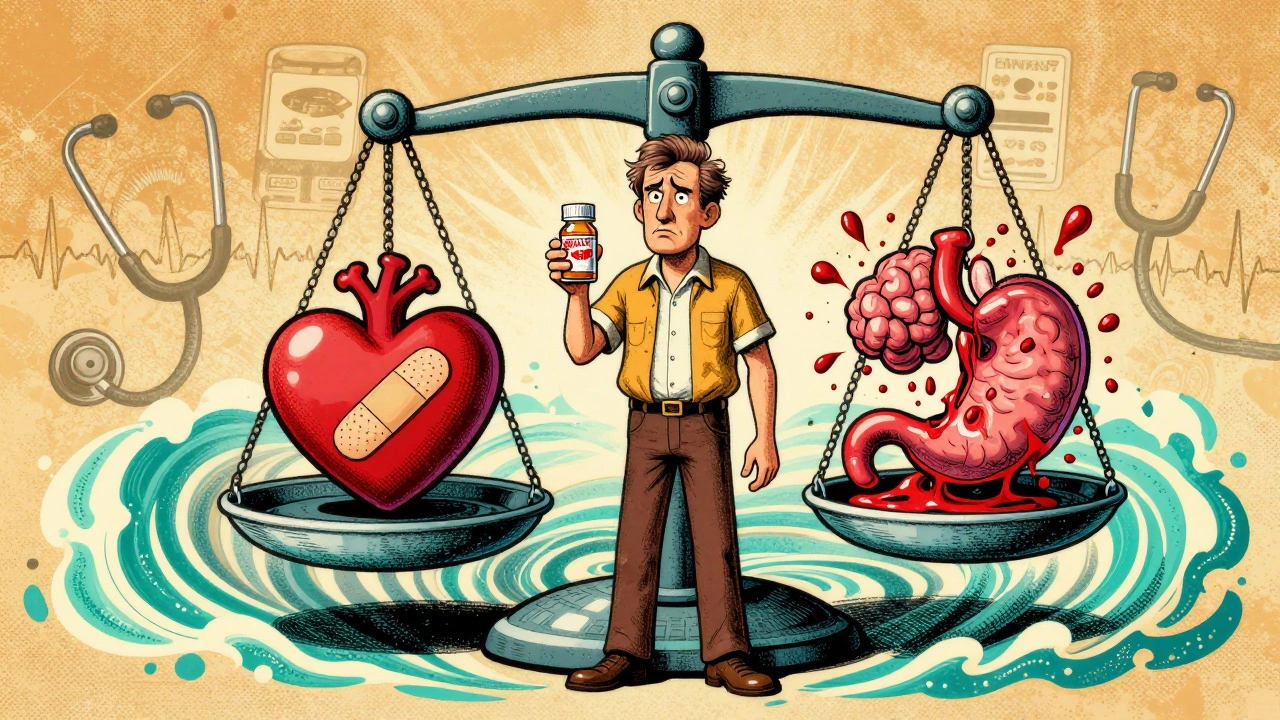
Aspirin’s Real Numbers: Benefits vs. Risks
Let’s put this in plain terms. For every 100 people like you who take low-dose aspirin daily for 10 years:
- 1 person might avoid a nonfatal heart attack
- 1 person might avoid a nonfatal stroke
- 2 people will have a serious bleeding event requiring hospitalization or a blood transfusion
That’s not a good trade. And the bleeding risk doesn’t go down with time-it goes up. The older you get, the more likely you are to bleed. That’s why guidelines now say: if you’re over 60, don’t start. If you’re already on it, talk to your doctor about stopping.
Aspirin’s benefit is strongest in people with diabetes and other risk factors. The American Diabetes Association still recommends aspirin for adults over 40 with diabetes who have at least one additional risk factor-like high blood pressure or smoking. But even here, the recommendation is cautious. It’s not automatic. It’s a discussion.
What About Family History?
“My dad had a heart attack at 58-I need aspirin.” This is the most common reason people give for continuing aspirin. But family history alone isn’t enough to justify it.
Genetics play a role, yes. But your own risk factors matter more. If you don’t smoke, your blood pressure is normal, your cholesterol is under control, and you exercise regularly, your personal risk may be low-even with a strong family history. Taking aspirin won’t cancel out your genes. It might just give you a bleeding ulcer.
Instead of relying on family history, get your 10-year risk calculated. That’s the only objective way to know if aspirin helps you.
Aspirin vs. Statins: Which One Actually Works?
Statins-drugs like atorvastatin and rosuvastatin-are now the cornerstone of heart disease prevention. They lower LDL cholesterol, stabilize plaque in arteries, and reduce inflammation. In large trials, statins cut heart attack risk by 25-37%. Aspirin? About 10-15%.
And statins don’t increase bleeding risk. They’re safer for long-term use in healthy people. If you’re at high risk for heart disease, you should be on a statin first. Aspirin, if used at all, is a secondary tool-not the main one.
Many people take both. That’s fine-if your doctor recommends it. But if you’re only taking aspirin and not a statin, you’re missing the bigger, more effective piece of the puzzle.
What If You’re Already Taking Aspirin?
If you’re over 60 and taking aspirin for prevention, don’t stop cold turkey. Talk to your doctor. Stopping suddenly can cause rebound platelet activation, which may slightly increase short-term risk. But that risk is far smaller than the long-term bleeding risk.
Your doctor will likely:
- Check your 10-year CVD risk
- Review your bleeding risk factors
- Assess whether you’re on other medications that increase bleeding (like NSAIDs or SSRIs)
- Discuss your personal values: Are you more afraid of a heart attack or a bleed?
If your risk is low and you have no clear benefit, stopping aspirin is the safest move. Many people feel better after stopping-no more stomach upset, fewer nosebleeds, less anxiety about bleeding.

What About Low-Dose vs. Regular Aspirin?
For prevention, the dose matters. The standard recommendation is 75-100 mg daily. That’s one baby aspirin (81 mg in the U.S.) or a quarter of a regular aspirin (325 mg). Higher doses don’t offer more protection-they just increase bleeding risk.
Don’t take 325 mg unless your doctor specifically tells you to. That dose is for heart attack recovery, not prevention.
Alternatives to Aspirin for Prevention
If you’re looking to reduce your heart disease risk, focus on what actually works:
- Take a statin if your risk is high
- Keep blood pressure under 120/80
- Get your LDL cholesterol below 70 if you’re high risk
- Exercise 150 minutes a week
- Stop smoking
- Manage diabetes tightly
- Eat more vegetables, whole grains, and healthy fats
These changes reduce your risk by 50% or more. Aspirin? At best, 10-15%. Lifestyle isn’t glamorous, but it’s proven.
Bottom Line: Aspirin Isn’t for Everyone Anymore
Aspirin isn’t a magic bullet. It’s a tool-with serious side effects. For most people, especially those over 60, it does more harm than good. The days of automatic daily aspirin are over.
If you’re under 60 and have high heart disease risk, talk to your doctor. Maybe aspirin makes sense for you. But don’t assume it does. Get your numbers checked. Understand your bleeding risk. Weigh the real numbers-not fear, not family history, not old advice.
If you’re over 60 and taking aspirin without a clear reason, it’s time to have that conversation. Your heart might be fine. But your stomach, your brain, your gut-those might not be.
Should I take aspirin every day to prevent a heart attack?
For most people, no. If you’re over 60, current guidelines say not to start. If you’re 40-59 and have a high risk of heart disease (10% or more in 10 years), you might benefit-but only if you don’t have a high bleeding risk. Always talk to your doctor before starting or stopping.
Is baby aspirin safe for long-term use?
Baby aspirin (81 mg) is the lowest effective dose for prevention, but it’s not risk-free. Long-term use increases your chance of stomach bleeding, brain bleeds, and other serious bleeding events-especially after age 60. The older you get, the higher the risk. For healthy adults over 60, the risks outweigh the benefits.
I have diabetes. Should I take aspirin?
If you’re over 40 and have diabetes plus one other risk factor-like high blood pressure, smoking, or kidney disease-your doctor may recommend aspirin. But it’s not automatic. Your bleeding risk must be low. Many people with diabetes are better protected with statins and tight blood sugar control than with aspirin.
What if my doctor still prescribes aspirin for prevention?
Ask why. Request your 10-year cardiovascular risk score. Ask about your bleeding risk. Ask if a statin would be more effective. Some doctors still follow old habits. You have the right to understand the evidence behind any recommendation. If your risk is low and you’re over 60, stopping aspirin is likely the safer choice.
Can I stop aspirin cold turkey?
If you’ve been taking aspirin daily for years, don’t stop abruptly without talking to your doctor. While the risk of rebound clotting is small, your doctor may recommend tapering or switching to another medication if needed. But if you’re taking it for primary prevention and have no heart disease, stopping is generally safe and often beneficial.
16 Comments
Robert Gilmore December 7, 2025 AT 14:46
So basically aspirin is now the new sugar? Everyone used to love it, now we’re told it’s poison lol
Robert Gilmore December 8, 2025 AT 21:39
My grandpa took aspirin daily since the 80s and still hikes every weekend 😅 maybe the docs are just overcomplicating things now?
Robert Gilmore December 9, 2025 AT 07:03
It’s terrifying how many people still cling to outdated medical advice like it’s gospel. The science is clear: aspirin for primary prevention is a relic of the pre-statins era. Continuing it without a clear risk profile isn’t precautionary-it’s reckless. People need to stop trusting anecdotes over data.
Robert Gilmore December 9, 2025 AT 15:45
I’m 58, have high cholesterol but no other risk factors. My doc ran the calculator and my score was 6.8%. She said ‘no aspirin, but let’s get you on a statin.’ I felt so relieved-finally someone listened to the numbers, not just the habit!
Robert Gilmore December 11, 2025 AT 03:57
My mother had a GI bleed at 72-after 15 years of daily aspirin. She’s fine now, but it was terrifying. I asked my doctor for the risk calculator last week. Scored 5.2%. No aspirin. No regrets. If your doctor pushes it without checking your score, ask for a second opinion.
Robert Gilmore December 11, 2025 AT 14:34
For anyone who says ‘but my dad had a heart attack!’-I get it. I lost my dad too. But here’s the thing: genetics aren’t destiny. I have a family history, but I exercise, eat well, and my LDL is 65. My doctor said aspirin wouldn’t add anything meaningful. Statins and lifestyle are the real heroes. Don’t let fear make you ignore the math.
Robert Gilmore December 12, 2025 AT 09:57
Aspirin is not the problem, the problem is doctors who don’t update their knowledge. I saw a cardiologist last month who prescribed aspirin to me without checking my risk score. I had to push back. This isn’t just outdated-it’s dangerous. We need better education for providers, not just patients
Robert Gilmore December 13, 2025 AT 19:47
It’s interesting how medicine keeps evolving-and how slow society is to let go of old rituals. Aspirin was never magic. It was a crude tool that filled a gap in a less advanced era. Now we have precision. We should treat prevention like we treat software updates: patch the old, install the new. Clinging to baby aspirin is like refusing to upgrade from Windows XP because ‘it worked fine’.
Robert Gilmore December 14, 2025 AT 00:26
I used to take aspirin because I thought it was ‘just a little thing’. Turns out, it’s a little thing with big consequences. Last year I had a stomach ulcer from it-no warning signs. Now I’m on a statin, my BP is perfect, and I feel better than I have in years. Sometimes the simplest change is the hardest to make.
Robert Gilmore December 15, 2025 AT 16:32
Aspirin for prevention? Nah. 🚫 I’d rather eat a salad than take a pill that might bleed me out. Statins, walking 10k steps, sleep, stress management-those are the real MVPs. Also, if your doctor still prescribes aspirin like it’s 2005, send them a link to the USPSTF guidelines. 🤓
Robert Gilmore December 17, 2025 AT 10:50
Of course the guidelines changed. Because now, doctors don’t want to be sued for not prescribing aspirin-they want to be sued for prescribing it. It’s not about science anymore. It’s about liability. And patients? We’re just the pawns in their legal chess game.
Robert Gilmore December 17, 2025 AT 14:19
Check your 10-year risk. Talk to your doctor. Don’t assume. Don’t fear. Act based on data.
Robert Gilmore December 19, 2025 AT 06:50
My mom’s doctor told her to take aspirin ‘because she’s a woman over 50’. I rolled my eyes so hard I got a headache. She stopped it last year. No more stomach burns. No more ‘should I take it today?’ anxiety. She says she feels like she finally got her health back. Turns out, the pill wasn’t helping-just haunting her.
Robert Gilmore December 21, 2025 AT 02:49
People still don’t get it. Aspirin isn’t a vitamin. It’s a drug. And drugs have consequences. The fact that millions took it daily without a second thought says more about our culture’s blind trust in pills than it does about medical science. We need to stop treating prevention like a vending machine-pop a pill, feel safe. Real health isn’t that simple.
Robert Gilmore December 21, 2025 AT 09:01
So if I’m 45, have high BP and smoke, but my score is 9.8%-do I take aspirin? Or not? The guidelines say ‘personal decision’-but that’s not helpful. What does ‘benefits outweigh risks’ even mean? Give me a number, not a philosophy.
Robert Gilmore December 22, 2025 AT 11:45
Actually, I just checked my score. 11.2%. Doc says aspirin makes sense. Took it today. Still feel weird about it. But at least now I know why.