
Why Your Insulin Injections Might Be Causing More Than Just Pain
If you’ve been injecting insulin for months or years, you might notice lumps under your skin, unusual bruising, or erratic blood sugar swings-even when your dose hasn’t changed. These aren’t just random annoyances. They’re signs of lipodystrophy and injection-related bruising, two common but often ignored complications that can wreck your diabetes control.
Up to 50% of people using insulin develop lipohypertrophy, the most common form of lipodystrophy. That’s half of all insulin users. And bruising? One study found nearly 66% of patients had visible bruising after injections. Yet most doctors don’t check injection sites during routine visits. If you’re struggling with unpredictable highs and lows, it might not be your insulin dose-it’s your injection technique.
What Lipodystrophy Really Looks Like (And Why It Matters)
Lipodystrophy isn’t one thing. It’s two opposite problems hiding under the same name: lipohypertrophy and lipoatrophy.
Lipohypertrophy is when fat builds up under the skin, creating soft, rubbery, raised lumps. These can be as big as a golf ball. They’re usually painless, which is why people keep injecting into them-thinking it’s less painful. But here’s the catch: insulin doesn’t absorb properly from these lumps. It’s slow, uneven, and unpredictable. That’s why your blood sugar spikes for no reason, or you get sudden hypoglycemia after a dose that normally works fine.
Lipoatrophy is the opposite. It’s when fat cells die off, leaving a shallow dent or indentation in the skin. This used to be more common with older insulin types, but it’s still seen today, especially with allergic reactions to insulin or preservatives. Unlike lipohypertrophy, lipoatrophy doesn’t cause erratic absorption-it just makes injections harder because the skin is thin and uneven.
Both conditions are caused by repeated injections in the same spot. The body responds to trauma by either packing on fat or breaking it down. Neither is dangerous on its own, but both sabotage your blood sugar control.
Why Bruising Happens-and Why It’s Not Always Harmless
Bruising from insulin injections is more common than most people realize. In one study of 1,370 patients, 901 had visible bruising. That’s over two-thirds.
Bruising happens when the needle hits a small blood vessel. It’s not the same as hitting a vein during a blood draw. This is a tiny capillary, and the bleed is minor. The area turns purple or blue and fades in a few days. But here’s what most people don’t know: frequent bruising is a red flag.
Studies show people who bruise often are also more likely to develop lipohypertrophy. Why? Because they’re probably pressing too hard on the injection pen, using the same spot repeatedly, or reusing needles. A dull needle tears tissue instead of slicing cleanly. Reusing needles also increases the chance of bleeding because the tip becomes bent or blunt after just one or two uses.
And if you’re injecting into a lipohypertrophic lump, you’re more likely to hit deeper vessels. That’s why bruising can be a warning sign-not just a cosmetic issue.
Where These Reactions Happen (And Why Your Belly Isn’t Safe)
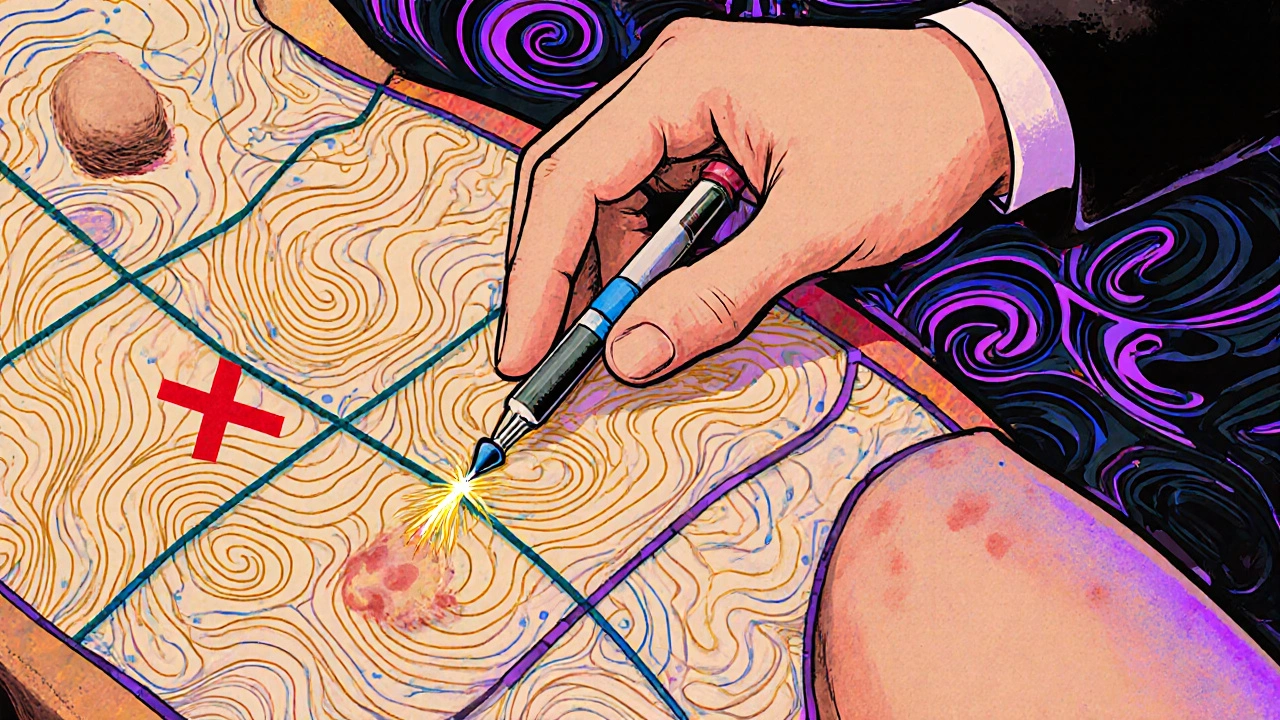
Most injections happen in the abdomen. That’s easy, accessible, and has a good fat layer. But here’s the problem: 78% of lipohypertrophy cases occur in the abdominal area. That’s because people get lazy. They stick to the same few inches around their belly button, rotating just a centimeter or two. It’s not rotation-it’s circling the same spot.
Thighs come second, with 22% of cases. Arms and buttocks are underused. That’s a mistake. Your body has plenty of space. The key is to treat your injection zones like a grid.
Use the full abdomen: left side, right side, above the hips, below the ribs. Then switch to thighs, then upper arms. Don’t stay in one area for more than a month. Even if you’re rotating, if you’re only moving 0.5 inches each time, you’re still hitting the same tissue over and over. You need at least 1 inch between injections. And don’t reuse a spot for 4 to 8 weeks.
How to Check Your Injection Sites (Even If You Can’t See Them)
Most people don’t know what to look for. They check for redness or swelling-signs of infection. But lipodystrophy doesn’t look like an infection. It’s not hot. It’s not tender. It doesn’t ooze. It’s just… there. A lump. A bump. A dip.
Here’s how to check:
- Take a warm shower first. Heat helps relax the skin.
- Use your fingers, not your eyes. Run your fingertips gently over each injection area.
- Feel for anything that’s firmer, bouncier, or raised compared to the surrounding skin.
- Look for depressions-shallow holes where the skin sinks in.
- Mark your findings with a pen or app. Take a photo every month.
Don’t wait for your doctor to check. Do it yourself. If you feel a lump, stop injecting there. Give it 6 to 8 weeks to recover. Injecting into lipohypertrophy makes it worse. It’s like pouring cement on a crack-it just gets bigger.
How to Fix It: The Simple Rules That Work
There’s no magic drug or cream to fix lipodystrophy. The only cure is time-and better technique.
Here’s what actually works:
- Use a new needle every time. Even if it doesn’t hurt, reuse increases bruising and tissue damage. A 32-gauge needle is thin enough for comfort and reduces trauma.
- Rotate systematically. Divide your injection areas into four zones: upper left, upper right, lower left, lower right abdomen. Use one zone per week. Move to thighs the next week. Then arms. Then back to abdomen-but a different quadrant.
- Don’t press hard. Hold the pen lightly. Let the needle do the work. If you’re pressing hard to make sure it goes in, you’re probably hitting blood vessels.
- Apply gentle pressure after injection. Don’t rub. Just press lightly for 5 to 10 seconds to stop bleeding. Rubbing causes bruising.
- Avoid long-acting insulins in problem areas. If you have a lump, don’t inject Lantus, Levemir, or Toujeo there. These insulins are more likely to cause lipohypertrophy than fast-acting ones.
People who follow these rules see results fast. One study showed a 47% drop in lipohypertrophy after just 3 months of structured training. Another user reported an 80% drop in unexplained low blood sugars after switching injection sites.
What Your Doctor Should Be Doing (But Probably Isn’t)
Most doctors don’t check injection sites. A survey found 61% of patients said their doctor never looked at their injection areas-even after years of insulin use.
That’s unacceptable. Your insulin isn’t working because of your dose. It’s working because of your skin.
Ask your doctor or diabetes educator to examine your injection sites at least once a year. If they don’t know how, bring a photo. Or better yet, ask for a referral to a certified diabetes care and education specialist (CDCES). They’re trained to spot these issues.
Some clinics now use ultrasound to map fat tissue. It’s not common, but it’s the most accurate way to confirm lipohypertrophy. If your blood sugar is erratic and you can’t figure out why, ask about it.
Technology Can Help-If You Let It
There are apps now that track your injection sites. InPen, Glooko, and others let you log where you injected and when. They show you a map of your skin and warn you if you’re hitting the same spot too often.
One 6-month trial with Glooko’s site-mapping tool reduced lipohypertrophy by 31%. That’s not small. That’s life-changing.
Insulin pumps like Medtronic’s MiniMed 780G now have built-in site tracking. They remind you where you last injected and suggest the next spot. If you’re on a pump, use it. Don’t ignore the alerts.
And don’t underestimate YouTube. Channels like “All About Diabetes” have step-by-step videos showing real people rotating sites. One viewer said their bruising dropped by 92% after watching and following along.
What Happens If You Ignore This
Ignoring injection site reactions doesn’t just make your blood sugar messy. It makes your diabetes harder to manage long-term.
People with lipohypertrophy have:
- 3.2 times higher risk of unexplained hypoglycemia
- 2.7 times higher risk of diabetic ketoacidosis (DKA)
- Up to 30% higher insulin doses needed to get the same effect
- A1c levels that stay stubbornly high-even with perfect diet and exercise
And the cost? Poorly managed lipodystrophy adds $1,850 per year to diabetes care. That’s because of more ER visits, more hospitalizations, more insulin waste.
This isn’t a minor issue. It’s a silent crisis in diabetes care. And it’s completely preventable.
Final Takeaway: Your Skin Is Part of Your Treatment Plan
Insulin doesn’t work in a vacuum. It works through your skin. And if your skin is damaged, your treatment fails.
You wouldn’t ignore a leaky fuel line in your car. Don’t ignore a damaged injection site in your body.
Check your skin every week. Rotate like your life depends on it-because it does. Use fresh needles. Don’t press hard. Avoid the lumps. And if you’re still getting bruises or erratic blood sugars? Look at your injection sites before you change your dose.
It’s not about being perfect. It’s about being aware. And awareness is the most powerful tool you have.
Can lipodystrophy go away on its own?
Yes, but only if you stop injecting into the affected area. Lipohypertrophy can shrink over 3 to 6 months with proper site rotation. Lipoatrophy may take longer-sometimes up to a year. The key is avoiding the spot entirely. Injecting into it again will make it worse.
Does bruising mean I’m injecting wrong?
Not always-but frequent bruising is a red flag. It usually means you’re reusing needles, pressing too hard, or injecting into the same spot too often. Try switching to a 32G needle, using a fresh one each time, and applying gentle pressure after injection instead of rubbing. If bruising continues, check for lipohypertrophy nearby.
Can I still inject into areas with lipoatrophy?
You can, but it’s not ideal. Thin skin with fat loss can make injections uncomfortable or uneven. The insulin may absorb faster than expected, increasing hypoglycemia risk. It’s better to avoid these areas and rotate to healthier skin. Over time, the tissue may recover, but it takes months.
Is lipohypertrophy dangerous?
Not directly. It’s not cancer or an infection. But it’s dangerous for your diabetes control. Insulin absorption becomes unpredictable, leading to high blood sugar, unexplained lows, and higher A1c. It also increases your risk of diabetic ketoacidosis and hospitalization. Treating it is critical-not optional.
Why do some people get lipodystrophy and others don’t?
It’s mostly about technique, not biology. People who rotate sites properly, use fresh needles, and avoid reusing the same small area rarely develop it. Those who inject in the same spot daily, reuse needles, or press hard are at highest risk. It’s not about insulin type or diabetes duration alone-it’s about how you use the needle.
Should I use a different insulin if I have lipodystrophy?
Not necessarily. Switching insulin types won’t fix the problem. The issue is your injection site, not the drug. But if you’re injecting long-acting insulin into a lump, consider switching the injection location to healthy tissue. Some people find that fast-acting insulins cause less tissue reaction, but technique matters more than the brand.
Next Steps: What to Do Today
- Look at your last 10 injection sites. Do you see any lumps or dents?
- Check your needle box. Are you reusing needles? Stop.
- Mark your calendar. Start a new rotation pattern next week-use a different body part each week.
- Download a free injection tracker app (like InPen or Glooko) and log your sites for 30 days.
- Ask your doctor to check your injection areas at your next visit. If they say no, ask for a referral to a diabetes educator.
Your skin holds the key to better blood sugar control. Don’t ignore it. Fix it. And your numbers will thank you.
14 Comments
Robert Gilmore October 29, 2025 AT 15:19
Just started checking my injection sites after reading this. Found a lump I didn’t even know was there. Stopped using that spot right away. My A1c’s been stuck at 8.2 for a year. Maybe this is why.
Robert Gilmore October 30, 2025 AT 20:43
Of course it’s your technique. You think insulin is magic? It’s a needle. You’re not a vampire. Use a new needle. Rotate. Stop being lazy. Simple.
Robert Gilmore October 31, 2025 AT 10:29
Thank you for this. I’ve been injecting in the same spot for 8 years because it ‘felt fine.’ Now I’m scared to look. But I’m gonna check tonight. 💪
Robert Gilmore November 1, 2025 AT 03:36
The pathophysiology of insulin-induced adipose remodeling is fundamentally a dysregulated wound-healing cascade mediated by chronic macrophage polarization toward an M2 phenotype. The fibro-adipogenic progenitor cells exhibit aberrant differentiation kinetics under persistent mechanical stress and inflammatory cytokine exposure-particularly IL-6 and TNF-α. This isn’t just ‘rotating sites.’ It’s epigenetic reprogramming of subcutaneous tissue microenvironments. You’re not just avoiding lumps-you’re interrupting a molecular feedback loop that’s been active since your first injection.
And if you’re using Lantus in a hypertrophic zone? You’re essentially creating an insulin reservoir with nonlinear pharmacokinetics. The absorption half-life isn’t 24 hours anymore-it’s erratic, biphasic, and unpredictable. That’s why your glucose swings don’t correlate with carb intake. The drug isn’t failing. Your tissue architecture is.
Ultrasound elastography is the gold standard for detection. But most clinicians haven’t seen a single case because they’re trained to treat glucose numbers, not skin morphology. We’ve turned diabetes into a lab result, not a whole-body condition.
And yes-lipoatrophy can be worse. At least lipohypertrophy is visible. Lipoatrophy hides. You inject into a depression, think it’s ‘normal,’ and get sudden hypoglycemia because the insulin hits capillaries directly. No fat buffer. No delay. Just a spike.
Stop thinking of this as ‘good hygiene.’ Think of it as tissue stewardship. Your skin isn’t a portal. It’s a pharmacokinetic organ. Treat it like one.
Robert Gilmore November 1, 2025 AT 08:14
Wait so you’re telling me I’ve been injecting into the same 2-inch circle on my belly for 5 years and that’s why my sugars are all over the place? I thought it was just stress or carbs. Huh. Guess I need to get better at this.
Robert Gilmore November 2, 2025 AT 08:35
One thing people miss: the needle angle matters too. 90 degrees is fine for most, but if you’re thin or have lipoatrophy, 45 degrees reduces depth and trauma. And don’t forget-some pens have shorter needles now. 4mm is enough. No need to go deep.
Also, if you’re using a pump, the infusion set placement is just as important. Same rules apply. Rotate like your life depends on it-because it does.
Robert Gilmore November 3, 2025 AT 16:56
You know what’s wild? I used to think bruising meant I was doing it right-like I was ‘getting it in deep.’ Turns out I was just tearing tissue. Now I use a fresh needle every time, no rubbing, and I barely bruise anymore. It’s not about force. It’s about precision. And patience.
Robert Gilmore November 4, 2025 AT 07:30
It is imperative that all insulin users undergo mandatory annual dermatological inspection of injection sites by a certified diabetes educator. Failure to do so constitutes a breach of the standard of care and constitutes medical negligence. The data is unequivocal. Lipohypertrophy is not a benign condition. It is a systemic failure of clinical oversight.
Robert Gilmore November 4, 2025 AT 23:33
So let me get this straight-you’re telling me the government and Big Pharma don’t want us to know that insulin absorption is messed up because they make more money when we need higher doses? And they don’t train doctors because they don’t want us to fix it ourselves? That’s why my A1c won’t drop even though I’m on 120 units a day?
I’ve been injecting in the same spot for 12 years because my doctor said it was fine. Now I’m supposed to believe this whole thing is about needle rotation? What’s next? Are my glucose meters rigged too?
Robert Gilmore November 5, 2025 AT 12:37
People in America think they can just inject anywhere and expect perfect control. In my country we rotate properly. We don’t wait until we’re in the ER for DKA to learn this. You think this is hard? Try doing it without insurance. Try doing it with three kids and no time. This isn’t a luxury. It’s survival.
Robert Gilmore November 5, 2025 AT 19:03
I live in New Zealand. We have a national diabetes program. Every patient gets a free injection tracker app and quarterly site checks by a nurse. No one here has lipohypertrophy. Why? Because we treat it like a public health issue. Not a personal failure.
Meanwhile, in the US, you’re expected to Google this on your own while paying $500 for a vial of insulin. This isn’t medicine. It’s capitalism.
Robert Gilmore November 6, 2025 AT 01:05
Wow. So the real problem isn’t your insulin. It’s your laziness. Your poor technique. Your ignorance. And you wonder why your A1c is high? Maybe you should stop blaming the system and start blaming yourself.
Robert Gilmore November 6, 2025 AT 09:59
THEY DON’T WANT YOU TO KNOW THIS. The FDA knows lipohypertrophy is caused by preservatives in insulin. They’ve known since 1998. But they let it continue because it keeps people buying more insulin. And the pens? They’re designed to make you reuse needles. The needles are too expensive. So they make them dull. So you bleed. So you think you need more insulin. It’s a SCAM. I’ve got the documents. I’ve got the emails. I’ll post them tomorrow.
Robert Gilmore November 6, 2025 AT 15:45
Wait-so you’re saying I can’t just inject wherever I feel like? Like, I have to plan it? Like, a schedule? That’s too much work. I just want to get it over with. Can’t I just use a different brand?