Taking a pill every day for years isn’t just a habit-it’s a lifeline. But for many people with chronic conditions like high blood pressure, diabetes, or rheumatoid arthritis, staying on track becomes harder over time. It’s not laziness. It’s not forgetfulness alone. It’s emotional fatigue, confusion, cost stress, and the slow erosion of motivation. The good news? There are proven ways to rebuild that connection between you and your meds-and they don’t require willpower alone.
Why Adherence Falls Apart After the First Few Months
Most people start their medication regimen with good intentions. But studies show that by the end of the first year, nearly half of those prescribed long-term drugs stop taking them as directed. Why? It’s rarely one thing. Complex regimens are a major culprit. Imagine needing to take five different pills at three different times of day, each with specific food rules or timing windows. That’s not just inconvenient-it’s mentally exhausting. A 2019 study of rheumatoid arthritis patients found that those who stuck with their meds had simpler routines and fewer daily doses. When doctors cut down the number of pills or switched to combination drugs, adherence jumped. Cost is another silent killer. Even with insurance, co-pays for specialty meds can hit $50 or more per month. For someone living paycheck to paycheck, that adds up fast. One patient in Sydney told me she skipped her statin every other month because she couldn’t afford it-until her pharmacist helped her apply for a government subsidy program. That’s not rare. The CDC estimates medication nonadherence costs the U.S. healthcare system $100-300 billion a year, mostly from avoidable hospital visits. Side effects, fear, and denial play their part too. Some people stop because they feel fine and think the drug isn’t doing anything. Others fear long-term side effects. A 2021 study on neurological patients showed that those who understood why their meds mattered were far more likely to keep taking them-even if they felt worse at first.The Five Coping Strategies That Actually Move the Needle
Research from a 2022 review of 15 studies across chronic conditions identifies five main ways people cope with long-term medication use. Not all work equally. Some help. Others backfire. Problem-solving / active coping is the clear winner. This isn’t just “I’ll set a phone alarm.” It’s actively identifying barriers and fixing them. For example: realizing you keep forgetting your afternoon pill because you’re always in the shower? Switch to a pill organizer with alarms. Can’t afford your medication? Talk to your pharmacist about generics or patient assistance programs. In 78% of studies, this approach led to better adherence. It works because it turns helplessness into control. Emotion-focused coping comes in second. This includes things like journaling about how you feel, using mindfulness to handle anxiety, or talking to a therapist about the stress of being “the sick person.” In 69% of studies, this helped. One patient with lupus said writing down her frustrations each week made her feel less alone. She started taking her meds because she didn’t want to let herself down-not because her doctor told her to. Seeking understanding means digging into your condition. Not just reading pamphlets, but asking questions: “What happens if I miss a dose?” “Why is this drug better than the last one?” “What are the real risks?” Patients who understand their disease are more likely to stick with treatment. A study in rheumatoid arthritis showed that those who could explain their meds to someone else had higher adherence scores. Support seeking is about leaning on others. Joining a patient group, talking to a friend who also takes daily meds, or even texting a family member to confirm you took your pill. The CDC found that patients who received team-based care-including pharmacists, nurses, and social workers-had an 89% adherence rate after 12 months. That’s nearly 15 percentage points higher than those who saw only their GP. Then there’s problem avoidance. This is the trap. Ignoring the problem, pretending you’re fine, delaying refills, or avoiding doctor visits because you don’t want to hear bad news. Half the studies showed this led to worse outcomes. In a few cases, it worked-usually when the person was in a stable phase of their illness and felt they didn’t need meds right then. But it’s risky. Relying on avoidance is like driving with your eyes closed hoping you won’t hit a wall.What Doesn’t Work (And Why)
Many common advice pieces miss the mark. “Just set a reminder!” doesn’t help if you’re overwhelmed by the number of pills. “Be more disciplined!” ignores the fact that discipline is a finite resource-it runs out. Pill organizers alone don’t fix adherence. I’ve seen patients with beautifully labeled boxes still skip doses because they didn’t understand why they were taking each one. A pill box is a tool, not a solution. Also, don’t assume older adults are more compliant. Yes, the rheumatoid arthritis study found older patients were more likely to stick with meds-but only if they had low complexity regimens and financial support. Many seniors skip pills because they’re afraid of interactions with other meds, or they can’t open bottles, or they don’t have transport to refill prescriptions. And don’t underestimate the power of shame. Many people hide nonadherence from their doctors because they fear being judged. That’s why team-based care works: pharmacists and nurses often build trust faster than doctors. They ask, “What’s been hard about taking your meds?” instead of “Why didn’t you take your pills?”
How to Build a Realistic, Long-Term Routine
Here’s how to turn coping strategies into daily practice:- Start with one change. Don’t overhaul everything. Pick the biggest barrier-maybe it’s cost, or timing, or side effects-and fix just that one thing first.
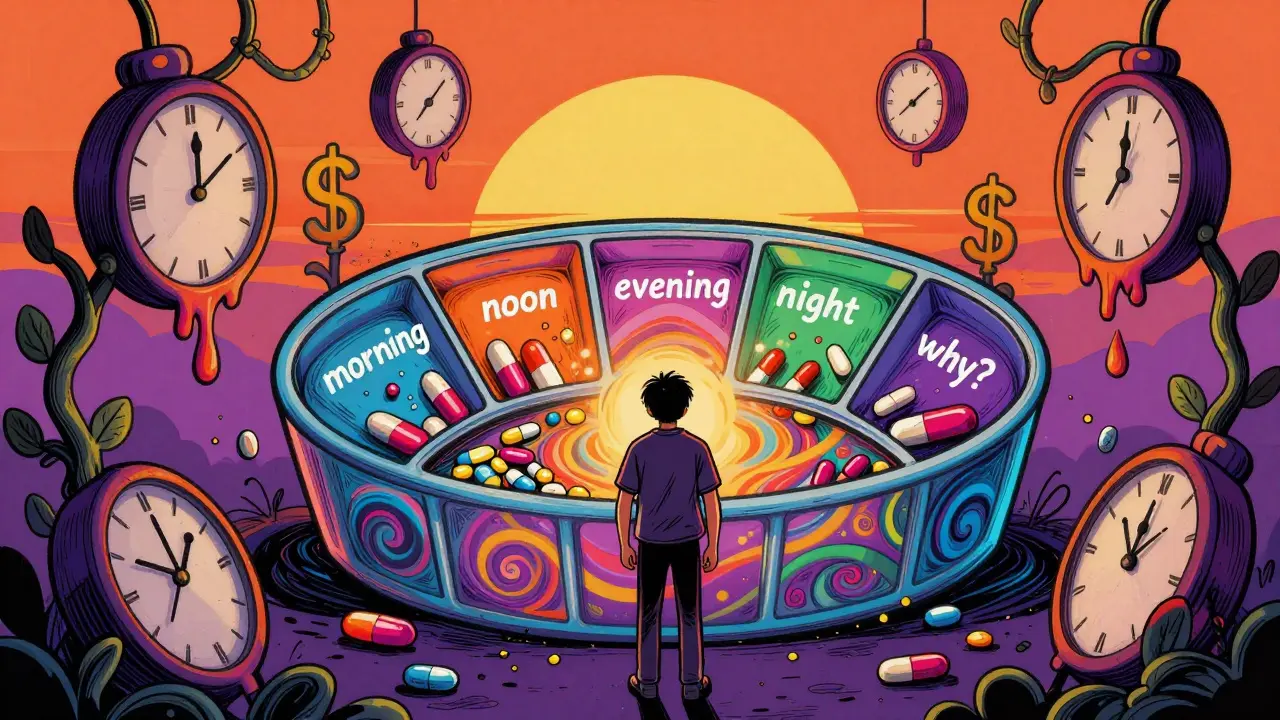
- Use a pill organizer with alarms. Choose one with compartments for morning, afternoon, evening, and night. Set two alarms: one to remind you, one as a backup 15 minutes later.
- Ask your pharmacist to simplify your regimen. Can your blood pressure pill be switched to a once-daily version? Can your diabetes meds be combined? Ask. Many doctors don’t think to ask you about this.
- Link meds to existing habits. Take your pill after brushing your teeth. Or right after your morning coffee. Habit stacking makes it automatic.
- Track your mood, not just your pills. Keep a simple log: “Took meds? Yes/No. How did I feel today? (1-5).” Over time, you’ll see patterns. Maybe you skip pills on stressful days. That’s useful info-not failure.
- Find your person. Someone who knows your routine and checks in. Not to nag-to support. A partner, a sibling, even a neighbor. You don’t have to do this alone.
When You Need More Help
If you’ve tried the basics and still struggle, don’t wait until you’re in crisis. Reach out. Pharmacists are your secret weapon. They can help you apply for medication assistance programs, explain side effects in plain language, and even deliver pills to your door in some areas. In Australia, programs like the PBS Safety Net cap your yearly spending on prescriptions. Ask your pharmacist how to enroll. If you’re feeling depressed, anxious, or hopeless about your health, talk to a counselor. Chronic illness and mental health are deeply linked. One study found that patients with untreated depression were twice as likely to stop their meds. Therapy isn’t a luxury-it’s part of your treatment plan. And if you’re worried about cost, don’t suffer in silence. Organizations like RxAssist.org (in the U.S.) or the PBS in Australia can help you get free or low-cost meds. You don’t need to be poor to qualify-many programs help people earning up to $60,000 a year.
The Bigger Picture: Why This Matters Beyond Your Own Health
Taking your meds isn’t just about avoiding a bad day. It’s about staying out of the hospital, keeping your job, being there for your kids, and not becoming a burden on the system. When adherence improves, hospitals see fewer emergency visits. Insurance costs drop. Medication waste decreases. One study found that for every $1 spent on adherence support, $3-$10 in healthcare costs were saved. It’s also about dignity. Living with a chronic condition is hard enough. You shouldn’t have to feel guilty for needing help. The goal isn’t perfection. It’s consistency. Even 80% adherence is better than 50%. And 80% is achievable-with the right tools and support.Final Thought: You’re Not Failing. The System Is.
Too often, we blame patients for not taking their pills. But the real failure is in a system that expects people to manage complex, expensive, emotionally draining routines with no support. You’re not broken. You’re human. The best coping strategies aren’t about willpower. They’re about design-designing routines that fit your life, not the other way around. And they’re about connection-having people who see you, not just your condition. Start small. Ask for help. Use what works. Your future self will thank you.Why do I keep forgetting my meds even when I set reminders?
Reminders help, but they don’t fix deeper issues. If you’re still forgetting, ask yourself: Are the pills too complex? Are you overwhelmed? Do you feel like the meds aren’t helping? Sometimes, forgetting is a sign you’re emotionally checked out. Try linking your pill to a daily habit like brushing your teeth. Or ask your pharmacist if you can switch to a once-daily version. You might also need emotional support-talking to someone who gets it can reignite your motivation.
Is it okay to skip a dose if I feel fine?
No-not without talking to your doctor first. Many chronic meds work behind the scenes. You might not feel symptoms, but your blood pressure, blood sugar, or inflammation levels could still be out of range. Skipping doses can lead to dangerous spikes or long-term damage. Even if you feel great, your body still needs the medication. If you’re wondering if you can stop, schedule a check-up-not a skip day.
How can I afford my medications if they’re too expensive?
You’re not alone. In Australia, the Pharmaceutical Benefits Scheme (PBS) caps how much you pay per script and per year. Ask your pharmacist to check if you’re eligible for the PBS Safety Net. In the U.S., RxAssist.org helps find patient assistance programs. Many drug manufacturers offer free or discounted meds if you meet income criteria. Also, ask if a generic version exists. Sometimes switching brands cuts costs by 80%.
Can my pharmacist really help me with adherence?
Absolutely. Pharmacists are trained to spot adherence issues and are often more accessible than doctors. They can simplify your regimen, explain side effects, help you apply for financial aid, and even call you to remind you about refills. Many pharmacies now offer medication therapy management services-free or low-cost-where they review all your meds and create a personalized plan. Don’t wait for your doctor to refer you. Walk in and ask.
I feel guilty for not taking my meds. Is that normal?
Yes, and it’s a sign you care. But guilt doesn’t fix anything. It just makes you feel worse. The goal isn’t perfection-it’s progress. If you missed a dose, don’t punish yourself. Just get back on track with the next one. Talk to your pharmacist or doctor about what’s making it hard. They’ve heard it all. You’re not disappointing them-you’re giving them the information they need to help you better.
Do coping strategies work for everyone?
Not the same way. What works for one person might not work for another. A 2019 study found that while active coping helped most people, its impact faded when adjusted for age, income, and disease duration. That means your background matters. A young person with limited income might need financial help more than a reminder app. An older person might need help opening bottles. The best approach is personalized. Don’t copy someone else’s system. Build your own based on your real life.
11 Comments
Robert Gilmore December 16, 2025 AT 02:59
It’s not about willpower. It’s about designing a life that doesn’t fight you every morning. I’ve seen people who take 12 pills a day and still show up for their kids, their jobs, their lives-not because they’re superhuman, but because they found one small anchor: a pill organizer next to the coffee maker, or a text from their sister at 7:30 a.m. Every system that works starts with one thing that’s easy. Not perfect. Just doable.
And the shame? It’s not yours to carry. The system made this hard. You didn’t fail. The system did.
Start with one pill. One habit. One person who asks, ‘How’d it go today?’ Not ‘Why didn’t you?’ That’s the difference between survival and thriving.
You’re not broken. You’re adapting.
And that’s courage.
Robert Gilmore December 17, 2025 AT 09:30
Adherence is a multivariate optimization problem constrained by cognitive load, financial capital, and health literacy. The 2022 meta-analysis referenced demonstrates that active coping strategies exhibit a statistically significant effect size (Cohen’s d = 0.78) when controlling for polypharmacy burden and socioeconomic status. The key insight is that behavioral compliance is not linearly correlated with patient motivation-it’s exponentially dependent on system-level simplification. Pharmacists are frontline cognitive architects: they reduce entropy in medication regimens by consolidating dosing schedules and identifying therapeutic redundancies. The $100B annual cost of nonadherence is not a public health crisis-it’s a systems engineering failure.
Stop blaming patients. Redesign the delivery architecture.
Robert Gilmore December 18, 2025 AT 00:24
bro i was takin my meds for 2 yrs straight then one day i just… stopped. not because i forgot. because i felt like the pills were makin me numb. like i was just existin, not livin. then i started journalin. just 3 lines a day. ‘took meds? yes/no.’ ‘how did i feel?’ ‘what did i do today?’
turns out i was skippin pills on days i felt empty. not because i was lazy. because i was sad.
talkin to my pharmacist changed everything. she gave me a generic version that cost $3. and asked me if i wanted to talk. not about my bp. about my life.
you’re not alone. even if it feels like it.
Robert Gilmore December 19, 2025 AT 13:45
Oh wow. A whole article about taking pills. Next up: ‘Coping Strategies for Breathing: What Actually Works.’
Let me guess-next week’s post is ‘The Hidden Truth About Drinking Water: Why You’re Probably Dehydrated (And How to Fix It).’
I mean, I get it. But at some point, isn’t this just… adulting? You take your meds. You don’t. You get sick. You go to the hospital. The end.
Why does this need 2000 words and a TED Talk vibe?
Robert Gilmore December 21, 2025 AT 09:49
Y’all are actin like people are too dumb to take pills. I’ve seen folks in this country skip their meds because they’re too lazy to get off the couch, then cry when they end up in the ER. You wanna know why? Because nobody’s holdin ‘em accountable. No one’s sayin, ‘Hey, you’re bein a dumbass.’
My uncle had diabetes. Took his insulin. Never missed. Why? Because his wife slapped him every time he tried to skip. Not mean. Just firm.
Maybe the problem ain’t the system. Maybe it’s people thinkin they deserve a free pass just ‘cause they’re sick.
Get tough. Get real. Stop coddlin.
Robert Gilmore December 22, 2025 AT 21:28
Who funds these studies? Big Pharma. The real reason people stop taking meds is because they start noticing the side effects-brain fog, fatigue, mood swings. They’re not ‘emotionally fatigued.’ They’re being poisoned slowly. The ‘adherence’ narrative is a marketing tool to keep you dependent. You think your blood pressure meds are helping? Or are they just masking symptoms while your liver dies?
Google ‘statin-induced myopathy.’ Read the FDA black box warnings. Then ask yourself: who really benefits when you keep taking these pills?
Don’t be a lab rat.
🌿 Go organic. 🌿
Robert Gilmore December 23, 2025 AT 05:49
I’m from Nigeria, and I’ve seen people in rural villages take their meds every day-even when they have to walk 10km to the clinic. Why? Because they know what happens if they don’t. No one’s handing them pill organizers. No one’s calling them to remind them. They do it because they’ve seen someone die from skipping.
Here in the US, we have so much: apps, subsidies, pharmacists on standby. And yet we feel entitled to skip because we’re ‘too busy.’
It’s not about willpower. It’s about perspective.
What would your grandmother from a village in Oyo do? She’d take that pill. Then she’d pray for you to do the same.
Robert Gilmore December 24, 2025 AT 05:42
Active coping isn’t just a strategy-it’s a mindset shift. You stop seeing yourself as a patient who needs to be managed, and start seeing yourself as a CEO of your own health. That means auditing your regimen like you’d audit a business: What’s the ROI on each pill? What’s the cost of skipping? What’s the system failure point?
I started tracking my mood and meds in Notion. After 3 months, I saw a pattern: I skipped my antihypertensive on weekends when I drank. So now? No alcohol on days I take it. Simple. Effective.
You don’t need more discipline. You need better data.
Track. Adjust. Repeat. That’s how you win.
Robert Gilmore December 25, 2025 AT 09:59
my mom took 8 pills a day for 15 years. never missed. not because she was perfect. because she had a ritual. coffee first. pill second. then she’d say out loud, ‘i’m doin this for my grandkids.’
that’s it. no app. no fancy organizer. just a reason that mattered more than the inconvenience.
we think we need tech. but sometimes we just need a little love tied to a habit.
you’re not a project. you’re a person. and you matter.
even on the days you forget.
Robert Gilmore December 27, 2025 AT 08:31
People who skip meds are making a moral choice. They’re choosing comfort over responsibility. It’s not a ‘system failure.’ It’s a character failure. You don’t get to be sick and then act like you’re above the basic expectations of adulthood. Take your pills. Show up. Be accountable. Or stop pretending you’re a victim.
My grandfather had heart disease. He took his meds. He didn’t whine. He didn’t blame the system. He just did what he had to do.
Some of us don’t need a therapist. We need a wake-up call.
Robert Gilmore December 28, 2025 AT 10:13
Y’all are missing the REAL issue. Big Pharma is secretly adding chemicals to make you dependent. The pills are designed to make you feel worse without them. That’s why you feel ‘emotionally fatigued’-it’s not your fault. It’s the lab. The government knows. The FDA knows. But they won’t tell you because they’re paid off.
My cousin’s doctor switched her to ‘generic’ and she started hallucinating. Coincidence? I think not. 🤫💊👁️
Ask yourself: Who profits when you keep taking these? 🤔
Stay vigilant. Stay skeptical. 🌐🔍